InterQual® Criteria features
Criteria are the clinical information the reviewer should consider when conducting reviews. Criteria comprise evidence-based clinical statements and rules for their application.
Depending on the product you select, criteria are organized in one of two formats:
Decision tree
Note: Applies to InterQual® LOC: Acute Adult and Acute Pediatric, LOC: Long-Term Acute Care, LOC: Inpatient Rehabilitation, LOC: Subacute and Skilled Nursing; InterQual® BH: Adult and Geriatric Psychiatry, BH: Child and Adolescent Psychiatry, BH: Substance Use Disorders; and InterQual® CP: Retrospective Monitoring and CP: Specialty Referral products.
In this format, the criteria are presented in a decision tree workflow in which you can see all the clinical statements and rules as you select criteria to conduct a review. Criteria include indications, criteria points, rules, and notes. You can select as many criteria points as you like or as recommended by your organization. However, only the minimum must be selected (as required by the rules) in order for criteria to be met.
Criteria in decision-tree format have these features:
-
Criteria points — refer to test results, medications, symptoms findings, or medical management. Criteria points support the reasons or indications; that is, they identify specific clinical elements that must be satisfied to justify the appropriateness of the intervention/service.
Criteria in a decision tree have top-level criteria points with one or more levels of underlying criteria points.
- Rules — specify how many of the underlying criteria points are needed to meet criteria, ensuring that reviewers apply criteria consistently. One, Both, and All are examples of rules.
-
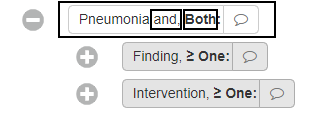
In LOC: Acute Criteria and CP: Specialty Referral Criteria, in some cases, to meet criteria, the patient must meet criteria for a criteria point with a rule AND for the underlying criteria. In the Acute Criteria example below, the patient must meet the Pneumonia criteria point and, per the rule, both the underlying criteria points, Finding and Intervention.
If you select criteria with this rule and you don't complete the selection, an indicator and text will appear to prompt you to finish the selection.
- Simple all — in LOC products (except Outpatient Rehabilitation & Chiropractic) and BH: Behavioral Health Criteria, where clinically appropriate, if you select a parent criteria point with a rule of All (or Both) that has only one level of underlying criteria points, then all of those underlying criteria points are automatically selected.
- Rule of One — for this rule, you can select only one underlying criteria point. If you select a second criteria point, an error message appears.
- Criteria status — the criteria status (initially, Criteria Not Met) is displayed as you conduct a review. If you select criteria points that meet the criteria, the status changes to Criteria Met. In Level of Care, Acute Adult or Pediatric criteria subsets, if you select criteria points that meet criteria for a specific level of care, the status indicates that level of care ( for example, Acute Met).
- Criteria notes — provide information such as explanations, definitions of medical terminology, information about a clinical condition, and specific reviewer instructions.
InterQual® Acute Criteria
InterQual Acute Criteria provide support for determining the medical appropriateness of hospital admission, continued stay, and discharge. Acute Adult Criteria address the Observation, Acute, Intermediate, and Critical levels of care. Acute Pediatric Criteria include these levels of care and additional levels of nursery care (Transitional Care, Newborn Level I, Special Care Level II, Neonatal Intensive Care Level III, and Neonatal Intensive Care Level IV).
Adult criteria are for review of patients ≥ 18 years of age. Pediatric criteria are for review of patients < 18 years of age.
Acute Criteria include these features:
Initial review
Some Acute Adult subsets include Initial review criteria. Initial review criteria are a level of care determination tool, intended to be used as real-time decision support in the emergency department to identify if observation or inpatient hospital-level services are warranted. They may help the reviewer assess whether a patient is appropriate for observation or inpatient status at the time a decision to hospitalize the patient is being made. Initial review criteria evaluate only data that are available at the time the decision is being made. This may include previously provided interventions or the results of laboratory, imaging, and other tests. Initial review may be appropriate when “bridge” or “holding” orders (e.g., “Admit to telemetry”) are in place. These orders are intended to address the patient’s needs until full treatment and medication orders are written..
Episode days
An episode day is a calendar day, which typically begins at 12:00 a.m. For evening admissions (e.g., after 6 p.m.), Episode Day 1 may represent the admission day (6 p.m.-11:59 p.m.) and the following hospital day. Within a subset, the number of episode days varies by condition; most address common comorbidities and complications associated with the primary condition. Each episode day includes only those levels of care that are clinically appropriate; an episode day may not include all levels of care.
Criteria subset redirection
Automatic redirection to a more appropriate subset or episode day within the current subset may be indicated in the content and/or in a pop-up message.
Abbreviations, symbols, and terms
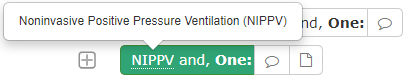
Select subsets in the Level of Care Acute Adult and Pediatric Criteria include abbreviations, symbols, or terms with a dashed underline. Moving the pointer over an underlined item expands it to provide the definition of the abbreviation or symbol, or full description of the term.
For example, the abbreviation NIPPV is underlined in this criteria point:
Care management information
Available for select level of care and Behavioral Health subsets and viewable with each episode day, Care management information outlines the expected clinical progress of the condition and provides suggestions for managing a patient if there are barriers to clinical progression. Care facilitation to the next appropriate level of care is also included. In some subsets, a section for Admission considerations has been included to identify the types of clinical findings/information that may be used to complete an admission review.
Utilization benchmark information
For additional information, refer to Understanding InterQual® benchmarks PDF).
InterQual content includes benchmarks for length of stay, percent paid as Observation, urine drug testing, and surgical site of service. The InterQual benchmark values are derived from a select set of de-identified claims data, representing 7 billion patient encounters. InterQual® benchmarks represent trends based on claims data and are not a reflection of evidentiary standards. Benchmarks are not intended to serve as treatment limits or substitute for clinical judgement. They are for informational use only.
Question and Answer (Q & A)
Note: Applies to InterQual® LOC: Home Care Q & A and LOC and Outpatient Rehabilitation & Chiropractic; InterQual® BH: Behavioral Health Services; InterQual® CP: Durable Medical Equipment, CP: Imaging, CP: Molecular Diagnostics, CP: Procedures, CP: Specialty Rx Non-Oncology, and CP: Specialty Rx Oncology; The ASAM Criteria®1 Navigator; Concert Genetics Navigator; and Medicare Content Navigator products.
In this format, criteria are presented in an interactive question-and-answer workflow that represents the same types of clinical statements and rules as those presented in a decision tree. As you conduct a medical review, your answers will lead you to the most appropriate drug, procedure, imaging study, test, service, or medical equipment. When you complete the medical review, the results are displayed on the Recommendations screen where you can choose among the recommendations, if any.
Questions and Recommendations
Answer choices are in one of the following formats:
-
Single-response: Choose one.
-
Multiple select: Choose all that apply.
The questions may also include criteria notes and rules that provide additional information and directions.
Each recommendation might have the following associated with it.
- Medical codes such as ICD, CPT®, and HCPCS.
- Rules that specify how some recommended services should be used with each other or should be mutually exclusive. For example, a Mutually Exclusive (ME) rule indicates that you can select only one of the recommendations.
- Utilization benchmark information is available for inpatient procedures in the InterQual® CP: Procedures product.
- A value associated with the recommendation, such as hour(s) per day, time(s) per year, or visit(s). For example, a Home Physical Therapy recommendation might indicate a number of visits within a given time frame, such as 6 visits within 2 weeks.
- Flags that provide explanatory text based on the results from the medical review. For example, a recommendation for a prescription medication might have an off-label flag. Specialty Rx Oncology drugs that are recommended for off-label use are based on the NCCN Drugs & Biologics Compendium NCCN Compendium®.
InterQual® CriteriaView
In products that have criteria organized in Q&A format, CriteriaView is a feature that enables you to view the criteria that leads to a recommendation for a specific procedure, imaging study, or other service. During a medical review, you select a specific recommendation(s) and then track that recommendation’s availability as you answer questions about clinical presentation. If your selected recommendation(s) remains available, you are led to a recommendation(s) for that service. However, if a selected recommendation becomes unavailable, you can see immediately which answer caused it to become unavailable. Additionally, you have the option to view remaining criteria and answer additional questions for that recommendation. The Recommendations screen provides results that show why criteria for your recommendation (requested intervention) were not met.
CriteriaView includes these main features:
- CriteriaView pane — available with the Medical Review Q&A workflow and the Book View Q&A workflow, enables you to view and track recommendations for a selected subset. When you begin a medical review, all possible recommendations are available for the subset. As you answer questions, the list of available recommendations reduces based on your answers so that only recommendations that are still clinically appropriate remain.
- Additional Criteria — available from the CriteraView pane and the Recommendations screen, enables you to view additional criteria and answer questions for recommendations that become unavailable. Answering the additional questions allows you to capture as much information as possible for the medical review.
- Recommendations/results — available in the Recommendations screen, the results show why a requested intervention was not recommended. It lists each clinical scenario for the recommendation and provides a comparison between your selections and the selections that lead to the recommendation.
- Review Summary — provides a complete picture of the review. In addition to the initial medical review questions and answers, it includes the additional criteria questions and answers that show why the requested intervention was not recommended.